Fax requested records to 866-305-6655. to ensure the medical records are indexed correctly, please attach the medical record request letter from humana for each claim. if you have questions or need further assistance, please call at 800-438-7885 (tty: 711). representatives are available monday through friday from 8 a. m. to 8 p. m. eastern time. Your private medical record is not as private as you may think. here are the people and organizations that can access it and how they use your data. in the united states, most people believe that health insurance portability and accountabil. When you need to file for medical reimbursement, this means you're submitting a claim for payment for services you've received. fortunately, if you're confused about the process, there are solutions. the following guidelines are for how to. Humana group medical plans are offered by humana medical plan, inc. humana employers health plan of georgia, inc. humana health plan, inc. humana health benefit plan of louisiana, inc. humana health plan of ohio, inc. humana health plans of puerto rico, inc. license 00235-0008, humana wisconsin health organization insurance corporation.
Appointment of representative form for appeals and grievances. if you are filing an appeal or grievance on behalf of a member, you need an appointment of representative (aor) form or other appropriate legal documentation on file with humana so that you are authorized to work with humana on his or her behalf. 3. patient date of birth: 8. claim control number: 4. member id: 9. total billed amount of claim: 5. member name: 10. provider name: 11. are you including medical records with your request?.
To ensure proper routing and a thorough and timely review of your dispute, please include a copy of the completed humana ppi medical record review dispute request form, pdf opens new window that was attached to the original findings letter, and any other documentation related to your dispute. (medical records, operative reports, or other documentation) necessary to support your request to your completed. claims reconsideration request form. 3. all claim reconsiderations must be submitted no later than sixty (60) calendar days from the receipt of the original eob. 4. provider will be sent an eob or determination letter indicating. Form ssa-561 request for reconsideration when we make a decision on your claim, we send you a letter explaining our decision. if you do not agree with our decision, you can appeal—that is, ask us to look at your case again. if you applied.
Medicalrecords management policy: get details on submitting medical records to the humana ppi department. post-payment review policy: find out about review processes. prepayment review policy: get an explanation of the prepayment review process. Claimreconsiderationform. instructions: please ensure the reconsideration request is fully completed and returned with all reconsiderations submitted without proper documentation and a completed claim form will delay review of the request. beneficiary name: _____ ms medicaid id:_____ mail to: conduent, attn: medical review, p. o. In evaluating your claim, the adjuster will request your medical records, and could ask for an independent medical examination (ime). updated by david goguen, j. d. as your personal injury case proceeds, the insurance adjuster will want to g.
Medical Forms Cancer Net
Grievance/appeal request form humana.
Humana offers healthcare providers up to 3 opportunities to dispute humana’s medical record review findings (levels one, two and three). dispute requests are reviewed by licensed or certified personnel who were not the individuals who made the initial findings. please submit all levels of disputes to the following address or fax number:. Asco cancer treatment and survivorship care plansasco developed two types of forms to help people diagnosed with cancer keep track of the treatment they received and medical care they may need in the future: a cancer treatment plan and a su. Request patient medical records, refer a patient, or find a ctca physician. call us 24/7 to request your patient's medical records from one of our hospitals, please call or fax one of the numbers below to start the process. to refer a patie. In order to request an appeal of a denied claim, you need to submit your request in writing within 60 calendar days from the date of the denial. this request should include: a copy of the original claim the remittance notification showing the denial.
Claims resources for providers humana.
Form Ssa561 Request For Reconsideration Social Security Administration
Forms For Wps Health Plan Providers Wps
Single Paper Claim Reconsideration Requestform
Complaint and appeal request note: completion of this form is mandatory. to obtain a review submit this form as well as information that will support your appeal, which may humana medical records request for claim reconsideration form include medical records, office notes, discharge summaries, lab records and/or member history (this is not an all-inclusive list) to the address listed on your. Please use one (1) reconsideration request form for each enrollee. date: provider manual beacon health strategies completion of the waiver request form. paper request for 3) administrative appeals (humana caresourcetm will process clinical appeals). 4) claims medicare reconsideration request form centers for medicare. Level i -request for reconsideration (attach medical records for code audits, code edits or authorization denials. do not attach original claim form. ) level ii claim dispute (attach the following: 1) a copy of the eop(s) with the claim numbers to be adjudicated clearly circled 2) the response to your original request for reconsideration. do.
Medical records management policy: get details on submitting medical records to the humana ppi department. post-payment review policy: find out about review processes. prepayment review policy: get an explanation of the prepayment review process. You may use this address to return the form: humana, grievance and appeal department. p. humana medical records request for claim reconsideration form o. box 14546. lexington ky 40512-4546. be sure to visit. humana. com, where you’ll find health, wellness, and plan information. Medical record review dispute request form. please complete and attach this form to your formal letter of dispute to ensure your documentation is. routed appropriately. be sure to include the original medical record review initial findings letter and. any other documentation that supports your dispute.

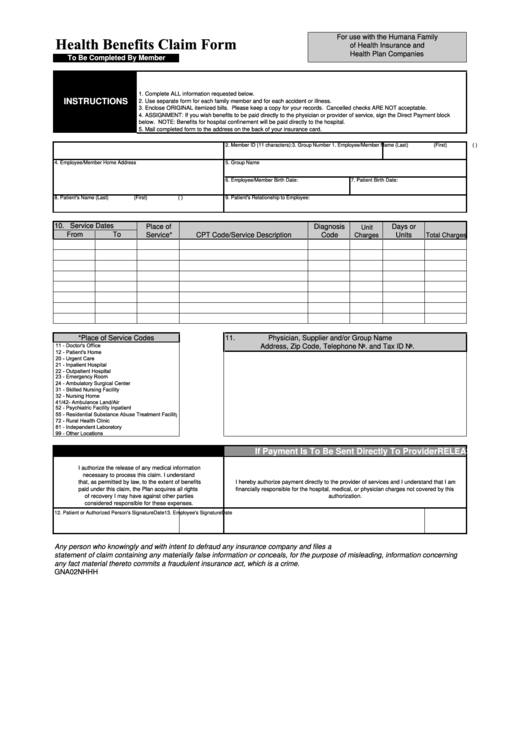
Mcrr 07/2016. provider reconsideration form. instructions: this form is to be completed by contracted physicians, hospitals, or other healthcare professionals to request a claim review for members enrolled in a commercial benefit plans administered by globalhealth.. mailing address: po box 2328 okc, ok 73101. attn:. Grievance/appeal request form gf-06_gar you may complete the form with information about the member whose treatment is the subject of the grievance/appeal. the appealing party does not have to return the form but we encourage its return because the form will help us resolve the appeal.
Default description use these forms if you are in dealing with a lawsuit-all written in plain-english by expert attorneys humana medical records request for claim reconsideration form at nolo. Medical record review dispute requestform. please complete and attach this form to your formal letter of dispute to ensure your documentation is routed appropriately. be sure to include the original medical record review initial findings letter and any other documentation that supports your dispute. fax materials to. 1-888-815-8912 or mail to:.


Patient referral authorization form providers should submit referrals and authorizations through provider self-service by logging into or registering for an account humana military only accepts a faxed form if the provider is unable to submit them electronically. Claims coding; payments; medical records; preauthorization & referrals. preauthorization lists; get details on how to request preauthorization for various tests and procedures, view online submission options and access state-specific forms. humana employers health plan of georgia, inc. humana health plan, inc. humana health benefit. It’s a patient’s right to view his or her medical records, receive copies of them and obtain a summary of the care he or she received. the process for doing so is straightforward. when you use the following guidelines, you can learn how to. The reconsideration request will be reviewed by parties not involved in the initial determination. in order to request a reconsideration, you need to submit your request in writing within the applicable time frame specified in state law. in addition to any other documents required by applicable law or state procedures, this request should include:.